
Medical Billing & Coding
Medical coding is the transformation of healthcare diagnosis, procedures, medical services, and equipment into universal medical alphanumeric codes. The diagnoses and procedure codes are taken from medical record documentation, such as transcription of physician's notes, laboratory and radiologic results, etc.
Medical coding professionals help ensure the codes are applied correctly during the medical billing process, which includes abstracting the information from documentation, assigning the appropriate codes, and creating a claim to be paid by insurance carriers.
Medical coding happens almost every time you see a healthcare provider. The healthcare provider reviews your complaint and medical history, makes an expert assessment of what’s wrong and how to treat you, and documents your visit. That documentation is not only the patient’s ongoing record, it’s how the healthcare provider gets paid.

How do you become a medical coder?
Successful medical coders know anatomy, physiology, medical procedures, and payer rules and policies. To become a medical coder, you must attend training via a coding-specific training program or college. Afterward, finding a job in the field is easier if you have a professional credential, such as SWANTECH.
There are several medical coding certifications available, depending on the area of the revenue cycle you wish to pursue. The baseline for most is the Certified Professional Coder (CPC), which certifies the coder’s ability to work in outpatient settings. Facility coders should pursue the Certified Inpatient Coder (CIC) for inpatient coding and Certified Outpatient Coder (COC) for hospital patients receiving in-and-out services. Here’s an infographic to help you choose the right hospital credential. There are several programs available both for online training on medical coding and physical medical coding training classes.
Accounts Receivable (AR) – Key Points
- Categorizing AR by aging buckets (0–30, 30–60, 60–90, 90+ days)
- Resolving pending issues such as coding errors, missing documents, or authorization problems
- Reworking and resubmitting claims promptly
- Creating preventive action plans to avoid repeat denials
- Following up until claim reconsideration is completed
- Improving collection rate and minimizing write-offs
- Maintaining healthy cash flow through timely recovery
- Insights into payer trends, denial patterns, and recovery performance
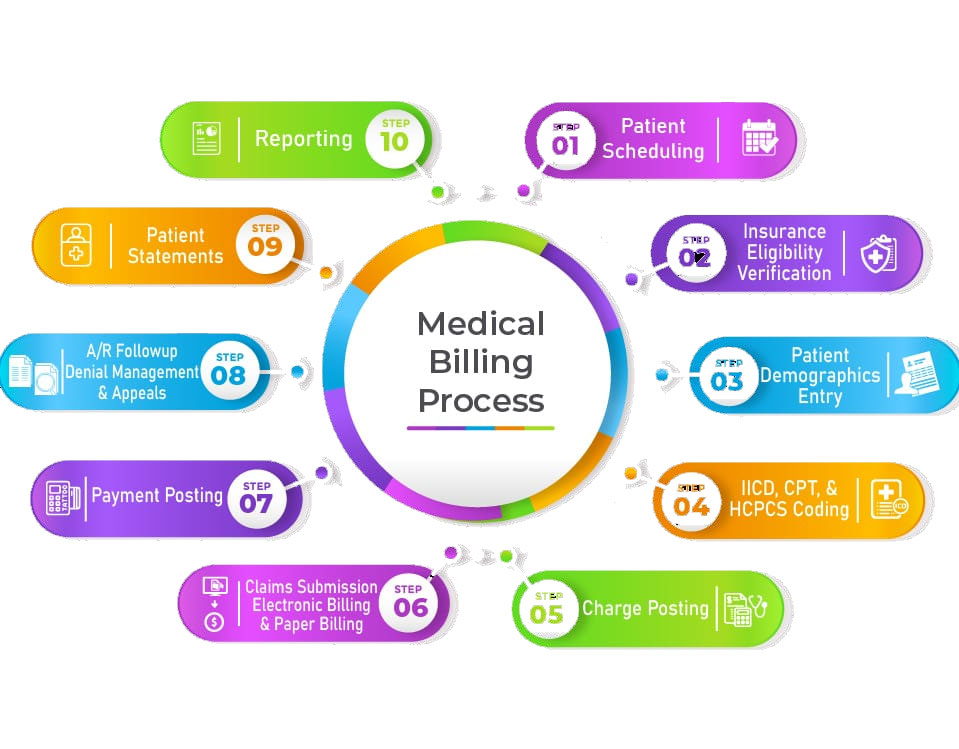
Revenue Cycle Management (RCM)
End-to-end management of the patient revenue journey from scheduling to final payment.
Accurate patient registration and insurance eligibility verification.
Efficient medical coding using ICD-10, CPT, and HCPCS standards.
Clean claim creation and timely submission to prevent delays.
Real-time tracking of claim status to reduce denials.
Compliance with HIPAA and payer-specific guidelines.
Detailed financial reporting and analytics to improve cash flow.
Reduction of AR days through proactive denial management.
Complete transparency with providers through regular performance updates.

We offer Premium Quality Training at very reasonable fees, making it accessible to all types of learners without compromising on quality.
